Antidepressants: drugs used to treat "depression." (NCIt) Mood-stimulating drugs used primarily in the treatment of affective disorders and related conditions. (MeSH)
Prescription drugs that are used to reduce the symptoms associated with "depression" - hopelessness, guilt, dejection, suicidal thoughts, difficulty concentrating, and disruptions in sleep, energy, appetite, and sexual desire. (Hockenbury 579) (They) elevate the mood of people suffering from depression. (Cardwell, 198)
First Generation Antidepressants: alleviate depression by increasing the availability of “norepinephrine” and “serotonin” in the brain. Can produce numerous side effects such as weight gain, dizziness, dry mouth and eyes, and sedation. (Hockenbury, 579)
Monoamine Oxidase Inhibitor (MAO Inhibitor): type of drug used to treat depression. It stops the breakdown of certain chemicals in the brain that help improve a person's mood. (NCIt) An “enzyme” that breaks down a class of “neurotransmitters” known as “monoamines.” In 1951, doctors and nurses… noticed that their patients taking a drug called ‘iproniazid’ (used to treat people with tuberculosis) seemed less lethargic and much happier than those not taking the drug. ‘Impramine,’ a drug developed initially to treat people with “schizophrenia,” was also found to relieve symptoms of depression, by blocking the “reuptake” of monoamines into “axon terminals.” Researchers discovered that monoamine oxidase breaks down and removes from the “synapses” two neurotransmitters: “noradrenaline” and serotonin. Without enough of these neurotransmitters, people experience symptoms of depression. Later, researchers found that iproniazid and imipramine also lead to an increase in the size and number of synapse in the hippocampus and the prefrontal cortex, the brain regions in which synaptic connections are damaged by stress and depression. (Kandel4, 68)
Tricyclics: substances used in the treatment of depression. These drugs block the (reuptake of norepinephrine and serotonin into “axon terminals” and may block some subtypes of serotonin and “histamine” “receptors.” However the mechanism of their antidepressant effects is not clear because the therapeutic effects usually take weeks to develop and may reflect compensatory changes in the “central nervous system.” (MeSH) Because tricyclics affect the “cardiovascular system,” an overdose can be fatal. (Hockenbury, 579)
Ketamine: (originally) a veterinary anesthetic, acts within hours in people with treatment-resistant depression. The effect of a single dose can last for several days. Also appears to reduce suicidal thoughts. Different from traditional antidepressants, it targets “glutamate,” not serotonin. Prevents the transmission of glutamate from one neuron to the next by blocking a glutamate receptor on the target (neuron). Since a receptor blocked by ketamine can’t “bind” glutamate, the neurotransmitter can’t affect the target (neuron). The discovery of ketamine has been hailed as the most important advance in depression research in the last half century. However, because it produces side effects such as nausea, vomiting, and disorientation, ketamine cannot be taken over the long term and therefore cannot replace the selective serotonin reuptake inhibitors. Instead, because of its rapid action, ketamine is used to lessen the risk of suicide during the approximately two weeks required for the (SSRI) drugs to take effect. (Kandel4, 69-70)
Second Generation Antidepressants: includes ‘trazodone’ and ‘buproprion.’ Although chemically different, these were no more effective than the first generation ones, and they turned out to have many of the same side effects. (Hockenbury, 579)
Wellbutrin: trade name for ‘buproprion.’ (Hockenbury, 579) Used to treat depression. It is also used as part of a support program to help people stop smoking. This medicine may be used to prevent depression in patients with “seasonal affective disorder,” which is sometimes called ‘winter depression.’ Bupropion is sold under different brand names for different uses. (PubMedHealth1)
Selective Serotonin Reuptake Inhibitor (SSRI): drug (that) increase concentrations of serotonin in the synapse by blocking the “reuptake” of serotonin. (However does) not act on noradrenaline. This finding led researchers to conclude that depression is related specifically to depletion of serotonin and not the depletion of noradrenaline. (Kandel4, 68) Selective serotonin reuptake inhibitors slow the process by which serotonin (a neurotransmitter), is reused by nerve cells that make it. This increases the amount of serotonin available for stimulating other nerves. (NCIt) Typically used as antidepressants. They alter serotonin availability. However, instead of altering the availability only at mood-crucial “receptors,” they alter serotonin availability everywhere. This results in side effects on sexual function and makes some people dizzy, sleepless, or fatigued. They also ignore genetic “variation” among people, so don’t work for all patients. (SAM, Oct/Nov 2007, 36)
Cymbalta: new antidepressant that is best classified as a ‘dual-reuptake inhibitor’ (because it) affects levels of both serotonin and norepinephrine. (Hockenbury, 579) Used to treat depression and anxiety. Used for pain caused by nerve damage associated with “diabetes.” Also used to treat “fibromyalgia” and “chronic pain” that is related to muscles and bones. (PubMed Health1) Editor’s note - generic name ‘duloxetine.’
Effexor: a dual-reuptake inhibitor. Affects levels of both serotonin and norepinephrine. (Hockenbury, 579) Used to treat depression. It is also used to treat “general anxiety disorder,” “social anxiety disorder,” and “panic disorder.” (PubMedHealth1) Inhibits neuronal reuptake of norepinephrine, “dopamine” and serotonin. (NCIt) Editor’s note - generic name ‘venlafaxine hydrochloride.’
Paxil: (a ‘third generation’) antidepressant drug that acts by prolonging the action of serotonin. Taken for the treatment of depression, "obsessive-compulsive disorder," panic disorder, "post-traumatic stress disorder," and some other anxiety disorders. (OxfordMed) A selective serotonin reuptake inhibitor with antidepressant and (anti-anxiety) properties. (NCI2) Editor’s note - generic name ‘paroxetine.’
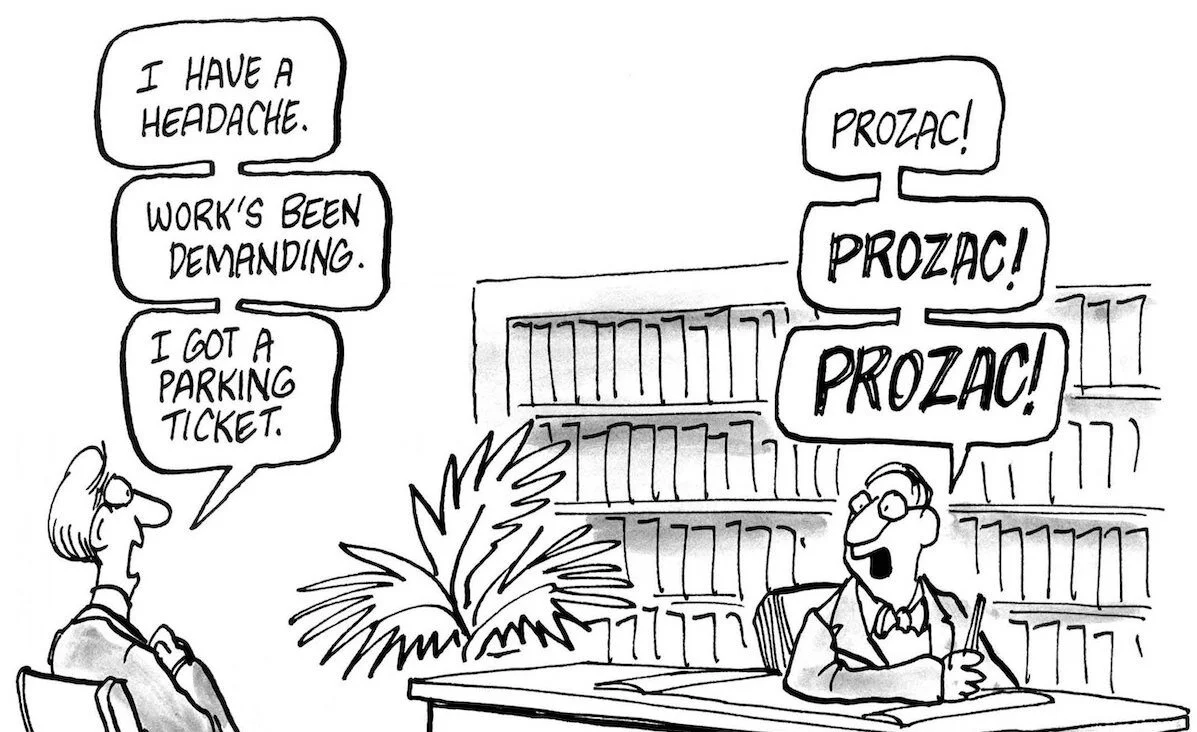
Prozac: first released selective serotonin reuptake inhibitor. Has less side effects than the 1st and 2nd generation drugs, but can have headaches, nervousness, difficulty sleeping, loss of appetite, and sexual dysfunction. By the early 1990’s, Prozac had become the best-selling antidepressant in the world. Trade name for ‘fluoxetin.’ (Hockenbury, 579) May help control anxiety by reducing the ability of inputs to the “amygdala” to activate fear circuits (pathways). Drugs like Prozac may reduce exaggerated fear and anxiety in psychiatric disorders by enhancing the ability of serotonin to facilitate "GABA” “inhibition" in the presence of elevated “cortisol.” (LeDoux, 63-64) In time, scientists realized that treating depression is more than a simple matter of flooding the synapses with serotonin. Boosting serotonin didn’t help all patients get better. Conversely, reducing serotonin didn’t consistently worsen symptoms in depressed people, nor did it produce depression in all healthy people. Moreover, antidepressant drugs, such as Prozac, increase serotonin very rapidly in depressed people yet people don’t show improvement in their mood or synaptic connections for weeks. (Kandel4, 69)
Zoloft: an antidepressant drug that acts by prolonging the action of serotonin. (OxfordMed) Used to treat depression, obsessive-compulsive disorder, panic disorder, post-traumatic stress disorder, and social anxiety disorder. It works by increasing the activity of a chemical called serotonin in the brain. (PubMedHealth1) Editor’s note - generic name ‘sertraline.’